Medicare Enrollment Periods
Leverage the experience of Brooks Insurance Group to weigh your Medicare coverage options.
When Can You Enroll in Medicare?
If you're approaching Medicare eligibility, it's important to understand when you can sign up for the coverage you need. Enrolling during the right window can help you avoid late penalties, coverage gaps, and unnecessary headaches. It's suggested to contact a broker prior to enrolling. Here's a breakdown of the key enrollment periods to be aware of:

1. Your First Opportunity: The Initial Enrollment Period (IEP)
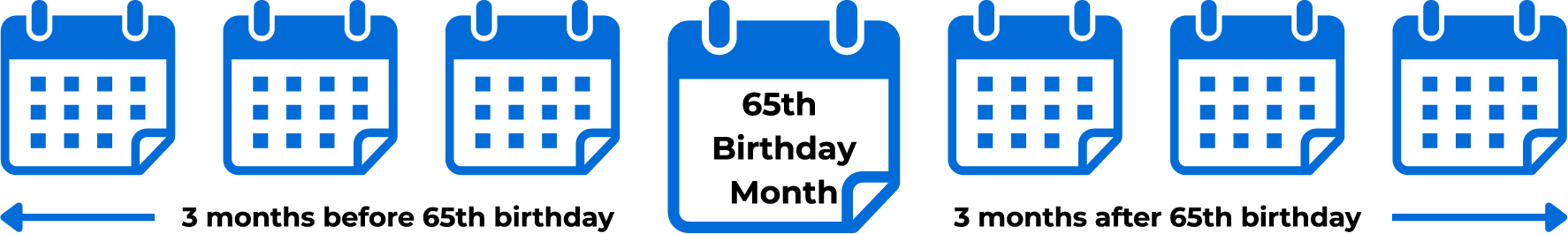
The Initial Enrollment Period is a 7-month window that surrounds your 65th birthday. It begins 3 months before, includes the month you turn 65, and continues for 3 months after.
During this time, you can enroll in:
- Medicare Part A (hospital insurance)
- Medicare Part B (medical insurance)
- Part C (Medicare Advantage) plans
- Part D prescription drug coverage
Signing up early helps ensure your coverage starts as soon as you're eligible.
2. Choosing an Advantage Plan: The Initial Coverage Election Period (ICEP)
If you're considering a Medicare Advantage (Part C) plan, your Initial Coverage Election Period is your first chance to enroll. This usually overlaps with your IEP, but if you delay enrolling in Part B, your ICEP is delayed too—it ends the month before your Part B coverage takes effect.
This period is important if you’re looking to combine hospital, medical, and often drug coverage into one plan.
3. Medigap Open Enrollment
Once you’re enrolled in Medicare Part B and age 65 or older, you get a 6-month Medigap Open Enrollment window. During this time, you can purchase a Medicare Supplement Insurance (Medigap) policy without undergoing medical underwriting.
After this period, you may be denied coverage or charged more based on health conditions..
4. Annual Enrollment Period (AEP)
Every year from October 15 to December 7, Medicare beneficiaries can:
- Switch from Original Medicare to Medicare Advantage (or vice versa)
- Join, drop, or switch a Part D prescription drug plan
- Change from one Medicare Advantage plan to another
Changes made during AEP take effect on
January 1 of the following year.
5. Medicare Advantage Open Enrollment Period (MA-OEP)
If you're already enrolled in a Medicare Advantage plan, you can make a one-time change between January 1 and March 31. This allows you to:
- Switch to another Medicare Advantage plan
- Disenroll and return to Original Medicare (with the option to join a Part D plan)
6. Missed Your First Chance? The General Enrollment Period (GEP)
If you didn’t sign up during your IEP, you can enroll in Medicare Part A and/or B during the General Enrollment Period, which runs January 1 to March 31 each year.
- Coverage starts July 1
- Late enrollment penalties may apply
This is a second-chance option—but it’s best to avoid the wait and potential penalties by enrolling on time.
7. Special Enrollment Periods (SEPs)
Certain life events may qualify you for a Special Enrollment Period. You might be eligible if:
- You lose employer or union coverage
- You move to a new area
- You’re released from incarceration
- You qualify for Medicaid or a Special Needs Plan
Timing for SEPs varies, but in most cases, you’ll have 2–3 months to enroll after the qualifying event.
Speak with a broker today to discuss Medicare Enrollment ➜